Spotlight on Clinical Trials: Shining a Light on Breast Cancer Disparities
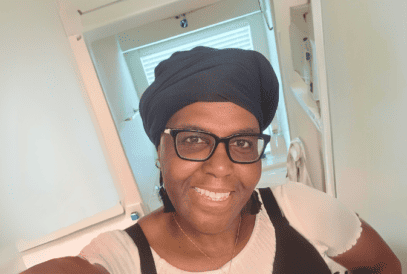
“In the Black community, there’s a stigma about treatment, clinical trials and research. We have to understand that there’s not enough data to help us if we get sick. There’s not enough data to create treatments that will help us. We need to participate in clinical trials.” Sharon Elmore-Anderson Patient Advocate Living with Metastatic IBC