Molecular Subtypes of Breast Cancer
How are molecular subtypes of breast cancer used?
Molecular subtypes of breast cancer are used mostly in research settings and are not part of a standard breast cancer diagnosis. So, the molecular subtype of your tumor is not part of your pathology report and is not used to guide your treatment.
Researchers are studying how molecular subtypes of breast cancer may be useful in planning treatment and developing new therapies.
Prognosis (chance of survival) and treatment decisions are guided mainly by tumor stage, tumor grade, hormone receptor status and HER2 status.
What are molecular subtypes of breast cancer?
The complex profile of each subtype is determined using molecular and genetic information from tumor cells.
Most studies divide breast cancer into 4 main molecular subtypes:
- Luminal A
- Luminal B
- Basal-like/triple negative
- HER2-enriched
These subtypes also appear in ductal carcinoma in situ (DCIS) [41].
There are many other less common molecular subtypes, including claudin-low and molecular apocrine types.
Luminal A
Luminal tumor cells look the most like cells of breast cancers that start in the inner (luminal) cells lining the mammary ducts.
Luminal A tumors tend to be:
- Estrogen receptor-positive (ER-positive)
- HER2 receptor-negative (HER2-negative)
- Tumor grade 1 or 2
About 40 percent of breast cancers are luminal A tumors [42-43].
Of the 4 main molecular subtypes, luminal A tumors tend to have the best prognosis (chance of survival), with fairly high survival rates and fairly low breast cancer recurrence rates [42-45].
Luminal B
Luminal tumor cells look like the cells of breast cancers that start in the inner (luminal) lining the mammary ducts.
Luminal B tumors tend to be ER-positive. They may be HER2-negative or HER2-positive.
Women with luminal B tumors are often diagnosed at a younger age than those with luminal A tumors [44,46].
Compared to luminal A tumors, luminal B tumors tend to have factors that lead to a poorer prognosis including [42-44]:
- Poorer tumor grade
- Larger tumor size
- Lymph node-positive
About 15-20 percent of breast cancers are luminal B tumors [42-43].
Women with luminal B tumors tend to have fairly high survival rates, although not as high as those with luminal A tumors [44-45].
Basal-like/triple negative
Basal-like tumors have cells that look similar to those of the outer (basal) cells surrounding the mammary ducts.
Triple negative breast cancers are:
- Estrogen receptor-negative (ER-negative)
- Progesterone receptor-negative (PR-negative)
- HER2-negative
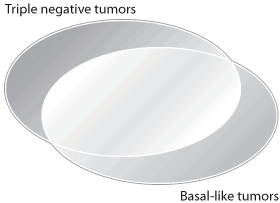
Most triple negative tumors are basal-like (see figure below).
About 15-20 percent of breast cancers are basal-like/triple negative [42-43,47-49].
These tumors tend to occur more often in [47-54]:
- Younger women
- People with a BRCA1 inherited gene mutation (if you’re diagnosed with TNBC, the National Comprehensive Cancer Network recommends you get genetic testing)
- Black, non-Hispanic Black and African American women (more on race/ethnicity and subtypes of breast cancer)
Triple negative tumors may also be more common among Hispanic women compared to non-Hispanic white women [49,55-56].
Learn more about BRCA1 inherited gene mutations.
Prognosis
Basal-like/triple negative tumors are often aggressive and have a poorer prognosis (lower chance of survival) compared to the ER-positive subtypes (luminal A and luminal B tumors) [43,45,48].
However, they can be treated effectively, and with new treatments for TNBC, prognosis is improving.
Learn more about triple negative breast cancer, including prognosis and treatment.
Learn about clinical trials for people with basal-like/triple negative breast cancers.
HER2-enriched
The molecular subtype HER2-enriched is not the same as HER2-positive and is not used to guide treatment.
Although most HER2-enriched tumors are HER2-positive (and named for this reason), many are HER2-negative [43].
HER2-enriched tumors tend to be [43-44]:
- ER-negative
- PR-negative
- Lymph node-positive
- Poorer tumor grade
About 10-15 percent of breast cancers are HER2-enriched subtype [42-43].
Women with HER2-enriched tumors may be diagnosed at a younger age than those with luminal A tumors [44,46].
HER2-enriched breast cancers that are HER2-positive can be treated with HER2-targeted therapies such as trastuzumab (Herceptin) and pertuzumab (Perjeta).
Race/ethnicity and molecular subtypes of breast cancer
Prevalence
Prevalence shows the proportion of people who have a breast cancer (or other health condition) at a given point in time. The prevalence of some molecular subtypes of breast cancer differ by race and ethnicity.
Basal-like/triple negative tumors appear to be more common among non-Hispanic Black and African American women (especially before menopause) compared to women of other ethnicities [47-49,51,54].
Triple negative tumors may be more common among Hispanic women compared to non-Hispanic white women [49,55-56].
Luminal A tumors may be more common among white women compared to women of other ethnicities [51,57].
Although the reasons for these differences are not clear, some factors (such as breastfeeding) may play a role [56,58-59].
Learn more about race/ethnicity and breast cancer.
Learn more about race/ethnicity and risk factors for triple negative breast cancer.
Prognosis
Higher rates of basal-like/triple negative tumors may explain, to some degree, the poor prognosis (chance of survival) of breast cancers diagnosed in Black, non-Hispanic Black and African American women [51,58,60-61].
Also, luminal A tumors, which have the best prognosis of the molecular subtypes, occur less often in Black women than in white women [51,57].
Learn about Susan G. Komen®’s work in advancing health equity.
Read our blogs:
|
Susan G. Komen partnered with Charles River Associates to publish the report, Inequities in Care and Treatment for Triple Negative Breast Cancer Patients, on the barriers to the care and treatment of TNBC. Read the full report. |
Updated 12/21/22


